All MCAT Biology Resources
Example Questions
Example Question #1 : Hormones
A person who has over-functioning pancreatic alpha cells may display what clinical feature?
Constipation
Decreased glucose levels
Increased digestion
Elevated glucose levels
Elevated glucose levels
The pancreatic alpha cells produce the hormone glucagon, which is responsible for stimulating gluconeogenesis and glycogenolysis. Gluconeogenesis is de novo formation of glucose, while glycogenolysis is the breakdown of glycogen into glucose. An increase in glucagon production through hyperactive alpha cells will result in increased blood glucose levels, at least temporarily. In a healthy individual, this will be combatted by an increase in insulin production from the pancreatic beta cell.
Example Question #1 : Hormone Origins And Targets
The activity of which of the following increases when parathyroid hormone is released into the blood stream?
T-cell maturation
The parathyroid gland
Osteoclasts
Osteocytes
Osteoblasts
Osteoclasts
Parathyroid hormone causes calcium to be released from the bone into the blood stream, raising blood calcium levels. Osteoclasts reside in bone and are responsible for resorbing the hydroxyapatite matrix, releasing sequestered calcium into the blood.
Osteoblasts counter osteoclasts, building the hydroxyapatite matrix and sequestering calcium stores. Osteocytes are mostly involved in signaling. The parathyroid gland releases parathyroid hormone, but is not affected by the hormone itself. T-cell mature in the thyroid, and are not affected by parathyroid activity.
Example Question #32 : Endocrine System
Which hormone is responsible for stimulating glucocorticoid release from the adrenal cortex?
Growth hormone
Prolactin
Thyroid-stimulating hormone
Adrenocorticotropic hormone
Adrenocorticotropic hormone
Adrenocorticotropic hormone (ACTH) is released from the anterior pituitary, and is responsible for stimulating secretion of glucocorticoids from the adrenal cortex. While cortisol is the most common and physiologically relevant glucocorticoid, others may also be synthesized. Adrenocorticotropic hormone release is stimulated by stress.
Example Question #2 : Hormone Origins And Targets
The hypothalamus uses two specialized types of neuron to stimulate the pituitary. Magnocellular neurons carry hormones directly to the posterior pituitary. Parvocellular neurons secrete hormones into the hypophyseal portal system, where they are delivered to the anterior pituitary.
The magnocellular neurons of the hypothalamus are responsible for secreting which hormone?
Dopamine
Thyrotropin-releasing hormone (TRH)
Thyroid-stimulating hormone (TSH)
Oxytocin
Oxytocin
The hypothalamus is divided up into two parts: the magnocellular neurons and the parvocellular neurons. The magnocellular neurons synthesize antidiuretic hormone (ADH) and oxytocin, which are then transported to the posterior pituitary for secretion. The parvocellular neurons secrete hormones such as corticotropin-releasing hormone (CRH) and thyrotropin-releasing hormone (TRH), which are released into portal circulation to be transported to the anterior pituitary.
Example Question #673 : Mcat Biological Sciences
Which of the following statements concerning hormonal transport is true?
Steroid hormones are able to move freely through the bloodstream
Pancreatic hormones are able to move freely through the bloodstream
The thyroid hormones are able to move freely in the bloodstream
All hormones require chylomicrons in order to move through the bloodstream
Pancreatic hormones are able to move freely through the bloodstream
The type of transport that a hormone will have through the bloodstream depends on the type of hormone. Peptide hormones are polar and can move freely through the bloodstream, while lipid soluble hormones require a carrier protein in order to move through the blood. The pancreatic hormones, glucagon and insulin, are peptide hormones. This means they can move through the bloodstream without a carrier protein.
In contrast, steroid hormones are derived from cholesterol and thyroid hormones are derived from tyrosine. Both of these hormone classes are lipid soluble, and require transport proteins to travel through the blood. The hormone-protein unit is known as a chylomicron.
Example Question #1 : Hormones
When calcitonin is released into the blood stream, the activity of which cell type is increased the most?
Erythropoietic stem cells
Hydroxyapatite cells
Osteocytes
Osteoclasts
Osteoblasts
Osteoblasts
Calcitonin is a hormone secreted by the thyroid in response to increased blood calcium levels. It counteracts high blood calcium by stimulating the deposit of calcium into bone. Osteoblasts are the most active cells in building the hydroxyapatite matrix of bone, and would be most stimulated by the release of calcitonin.
Osteocytes are matured osteoblasts in the bond interior, and are more active in signaling and regulation than bond formation. Osteoclasts counteract osteoblasts and break down bone, usually in response to parathyroid hormone. Hydroxyapatite is the crystalline matrix encasing the bone cells, but is not a type of cell itself. Erythropoietic stem cells reside in the bone marrow and produce blood cells, but are not involved in calcium regulation.
Example Question #1 : Hormones
Type I diabetes is the result of an immune-mediated destruction of the beta cells in the islets of Langerhans in the pancreas. Which hormone would be expected to be elevated in type I diabetes?
Somatostatin
Glucagon
Insulin
Oxytocin
Glucagon
The first key to understanding this question is remembering that beta cells in the pancreas are responsible for secreting insulin. If the beta cells are destroyed, then insulin levels are low. Insulin and glucagon act in opposite ways to keep the concentration of blood glucose in the normal range, providing a negative feedback loop. Insulin inhibits glucagon, and glucagon inhibits insulin. If insulin is low, then glucagon will not be inhibited and will be produced at higher levels than normal.
Example Question #1 : Hormones
Type II diabetes results from prolonged overstimulation of the pancreatic beta cells as a result of obesity and chronically elevated glucose levels. After the beta cells have been overactive for an extended period of time, they begin functioning poorly and the person is considered diabetic. In a type II diabetes, what are the expected levels of insulin and glucagon with respect to normal values?
Insulin levels will be low and glucagon levels will be low
Insulin levels will be elevated and glucagon levels will be low
Insulin levels will be low and glucagon levels will be elevated
Insulin levels will be elevated and glucagon levels will be elevated
Insulin levels will be low and glucagon levels will be elevated
Type II diabetes results from an eventual lack of function of the pancreatic beta cells. The first step to this problem is remembering that the beta cells produce insulin. If the beta cells do not function, insulin levels will be decreased. The second step to this problem is remembering that insulin and glucagon have contrasting actions in the regulation of blood glucose levels. They act in a negative feedback loop: insulin inhibits glucagon release, and glucagon inhibits insulin release. If insulin levels are low, then glucagon will no longer be inhibited. As a result, we would observe low levels of insulin and elevated levels of glucagon.
Example Question #1 : Hormone Origins And Targets
Which of the following is NOT a direct effect of the anterior pituitary?
Bone growth
T4 production
Ovulation
Milk production
Water retention
Water retention
Milk production is influenced by prolactin (produced in the anterior pituitary). Bone growth is influenced by growth hormone (produced in the anterior pituitary). Ovulation is controlled by luteinizing hormone and follicle-stimulating hormone (both produced in the anterior pituitary). T4, a thyroid hormone, is controlled by thyroid-stimulating hormone (produced in the anterior pituitary). Water retention, on the other hand, is controlled by antidiuretic hormone (produced in the hypothalamus and released by the posterior pituitary).
Example Question #661 : Biology
Scientists use a process called Flourescent In-Situ Hybridization, or FISH, to study genetic disorders in humans. FISH is a technique that uses spectrographic analysis to determine the presence or absence, as well as the relative abundance, of genetic material in human cells.
To use FISH, scientists apply fluorescently-labeled bits of DNA of a known color, called probes, to samples of test DNA. These probes anneal to the sample DNA, and scientists can read the colors that result using laboratory equipment. One common use of FISH is to determine the presence of extra DNA in conditions of aneuploidy, a state in which a human cell has an abnormal number of chromosomes. Chromosomes are collections of DNA, the totality of which makes up a cell’s genome. Another typical use is in the study of cancer cells, where scientists use FISH labels to ascertain if genes have moved inappropriately in a cell’s genome.
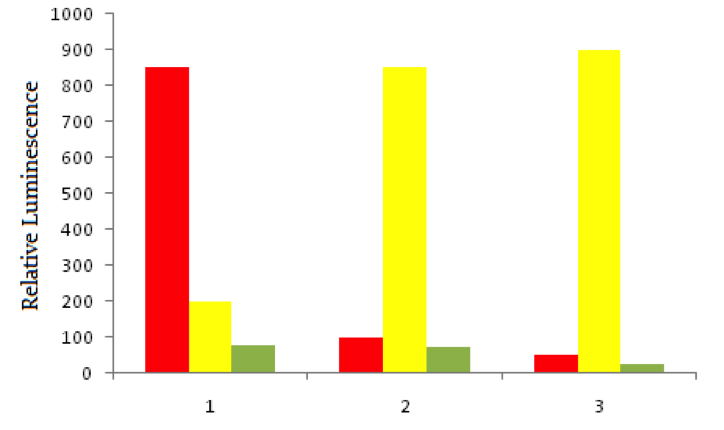
Using red fluorescent tags, scientists label probe DNA for a gene known to be expressed more heavily in cancer cells than normal cells. They then label a probe for an immediately adjacent DNA sequence with a green fluorescent tag. Both probes are then added to three dishes, shown below. In dish 1 human bladder cells are incubated with the probes, in dish 2 human epithelial cells are incubated, and in dish 3 known non-cancerous cells are used. The relative luminescence observed in regions of interest in all dishes is shown below.
Aneuploidy can also affect some fertilized zygotes after abnormalities in fertilization or gametogenesis. Aneuploid zygotes are typically spontaneously aborted before a pregnancy comes to term. A normal zygote binds to uterine endometrium while it is at its thickest, supported by progesterone secretion from which of the following?
Hypothalamus
Posterior pituitary
Corpus luteum
Anterior pituitary
Graafian follicle
Corpus luteum
The corpus luteum forms after ovulation, when a pregnancy would be most expected. The corpus luteum secretes progesterone, which maintains the endometrium for potential implantation.
All MCAT Biology Resources




